Hip Surgery 101. I get questions often about what exactly Hayes is having done on his hips. So, I’m going to try and explain from a parent’s perspective what hip surgery actually entails and what we have learned along the way. Including some post-op tips, what to look for and what to expect for getting through the 6-8 weeks of the spica cast phase. Check out previous Hospital Life post and Tips to Prepare for Hospital Life for more information too.
Hayes is on round two of hip surgery. In 2017 he had bilateral (both right and left side) femoral osteotomies — hold tight, I’ll explain what the heck I’m talking about. The main reason for needing the initial surgery was to alleviate pain due to hip dislocation or subluxation. Basically the head of the thighbone (femur) is coming in and out of its socket in the hip bone (pelvis). You might question how his hips became dislocated when he doesn’t walk, and that’s a fair question. It is attributed to his Cerebral Palsy (CP). Cerebral Palsy (more info here) is caused by injury or damage to the developing brain and is unique to each individual, but causes abnormal muscle movement and coordination. Therefore, his muscle tone, i.e. muscle activity at a passive or involuntary state, is abnormal. Muscle tone can be very “high” or hyper and tense and it can be “low” or hypo and weak, or both — which is what Hayes has. This abnormal tone puts stress on the hip joint affecting bone development and stability issues leading to displacement. Because the underlying problem is the CP and atypical muscle tone, there is always possibility of repeat surgery with growth. It is a neuromuscular hip dislocation, meaning caused by abnormal pull of spastic hip muscles, not injury or trauma. So the key is to try and manage the muscle tone and spasms and that’s a whole other ball game.
Definitions
Please reference International Hip Dysplasia Insitute (here) for more information.
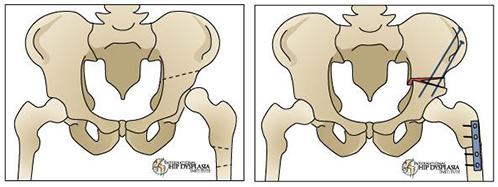
Osteotomy is a surgical procedure that involves cutting and reshaping of a bone to shift into better alignment.
Pelvic osteotomy involves reshaping a shallow hip socket so that it accommodates the ball of the hip joint. This is done to correct a hip socket that is too shallow or misshapen. Pelvic Oseotomy BCChildren’s
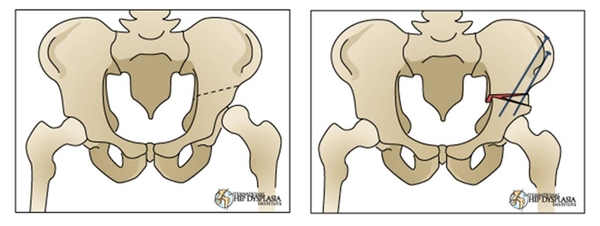
Femoral osteotomy involves reshaping and usually shortening the upper end of the thigh bone, the femur, to better align into the hip socket.
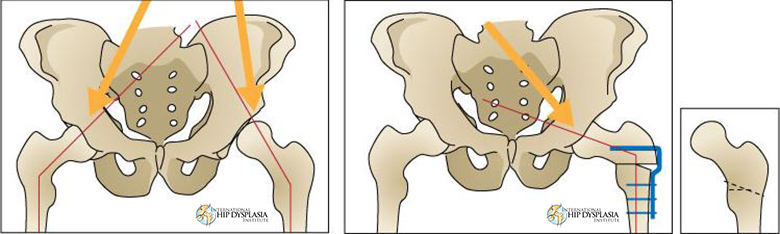
Open Reduction, Pelvic Osteotomy, Femoral Shortening and Varus Osteotomy. Open Reduction is where the broken bone is exposed by surgery and moving the tissue around it. This is the main combination of procedures Hayes had done — triple pelvic osteotomy.
Spica Cast
Spica casts are used to keep the femur and pelvis, basically the entire upper part of the leg, still or immobilized for healing. It includes one or both legs as well as the waist. Reference IHDI, Open Reduction, Spica Cast and OrthoKids – Spica Cast for additional information and siting.
We did not have a spica cast after our first hip surgery. He was much smaller and the procedure was not as extreme, so we came home with a foam wedge to keep his legs abducted (open). This procedure was much more complex, so the cast was needed. To say I was a little intimidated would be an understatement.
This time he ended up with a bilateral spica cast. I wasn’t expecting it, but they needed the additional stabilization. Since he just had the right hip repaired, they didn’t want him to compensate because of cast in turn compromising what they just fixed. The reason we got away with only having one leg casted during round one was because they knew the other hip was going to be operated on relatively soon. I’m missing that one-legged champ cast now. There is not much room for error in the diapering area this go around.
What to watch for with Spica cast
Bring up any concerns or areas you feel need to be addressed before you leave the hospital. It will make life a lot easier once you’re home. We had to make quiet a few adjustments to trim down the cast, in and out of the hospital.
- Check and feel around all edges, nooks and crannies of cast for sharp edges that may need to be trimmed down or padded.
- Look for pressure points in different positions. While laying down, the cast my put pressure on one spot, such as the shin, but in wheelchair the pressure could be around ribs or back of legs.
- Watch for circulation issues in these positions as well. Swelling, discoloration, etc.
- Keep an extra eye on the heels for breakdown. “Floating heels” are best to avoid pressure.
- Make sure there is ample room around G-tube, diapering area and ribs.
Wheelchair Accommodations
Many wheelchairs need adjustments made to accommodate the cast and new positions. This can include removing and adding different hardware. Arm and feet rest, lateral supports, and head rest may need a total makeover. The physical therapist and equipment vendors will help figure out what options will best accommodate before you go home. You all may have to get creative with padding and support. Think outside of the box — velcro, pool noodles, foam padding, pillows, straps, etc. This is really where the therapist shine. They see a lot of kiddos so they have a few tricks up their sleeve, lol.
Diapering
This was probably the biggest learning curve and the most intimidating. Incontinence issues are a major concern on a normal day, so add in the cast and it can be overwhelming. There is a lot of poop and pee that’s going to happen during the next six weeks so it’s important to figure out what works best to contain all the things and keep cast as clean as possible.
Double diapering and rolling will be your new forte. The key is using a smaller diaper under the cast and tucking it in the front and back of cast. Then use a second bigger diaper to go over the cast. It will be a two-person job at first. One to roll and hold and other to do cleaning and diapering, but you’ll find your groove soon. The cast is holding everything is place, so try not to worry about messing something up when you’re rolling them around and transferring.
I hope this information is helpful and can alleviate a little stress about surgery. I felt like I was totally winging it the first go around and would have loved some first-hand tips. It is a big undertaking, but knowledge is power in these situations. So, do your homework, ask the questions and speak up when you’re concerned. You know your child best. The doctors are the professionals for surgery, but you are the expert on your child. You know how they sit, how they breathe, their posture, what works and what doesn’t. Be the advocate they need when they can’t speak up for themselves. Remember to take a step back, give yourself some grace and let your faith be bigger than your fear. Thanks for checking in.
Emily




Could there be any more to deal with and accomplish? Thank you nurses, therapist and mom and dad. Always alert and ready. Cheering for all of you.